The International and Multi-Regional Membership Center of Latinos in the USA
Welcome to you all!




Special Article: Heroin Abuse In America & Statistics By Ethnicity

PuraVidaCommunity

Introduction and History
Opium, the first opioid, is derived from the sap of opium poppies, whose
growth and cultivation dates back to the ancient civilization of
Mesopotamia around 3400 BC. Opium was initially used by Egyptians
and Persians, eventually spreading to various parts of Europe and to
India and China. During the 18th century, physicians in the U.S. used
opium as a therapeutic agent for multiple purposes, including relieving
pain in cancer, spasms from tetanus, and pain attendant to menstruation
and childbirth. It was only towards the end of the 18th century that
some physicians came to recognize the addictive quality of opium.
In 1805, morphine and codeine were isolated from opium, and morphine was used as a cure for opium addiction
since its addictive characteristics were not known. Morphine’s use as a treatment for opium addiction was
initially well received as morphine has about ten times more euphoric effects than the equivalent amount of
opium. Over the years, however, morphine abuse increased.
Heroin was synthesized from morphine in 1874 by an English
chemist, but was not produced commercially until 1898 by
the Bayer Pharmaceutical Company. Attempts were made to
use heroin in place of morphine due to problems of morphine abuse. However, it turned out that
heroin was also highly addictive, and was eventually classified as an illegal drug in the United States.
Today, heroin in the United States comes mostly from Southeast Asia, Southwest Asia, Latin America
and Mexico. It is typically sold in a white or brownish powder form or as a black sticky substance
known as “black tar” heroin (black tar from Mexico is the most common form of the drug in Arizona).
Heroin found on the streets is usually mixed with other drugs or substances such as sugar, starch,
powdered milk, talc, baking soda, caffeine, cocaine, or quinine, though some reports indicate that
pure forms of heroin are becoming more widely available.
History of Heroin
Heroin, which is a very popular drug of choice in the American drug culture today, is not a new drug
that just showed up in the late 1960’s, nor are its negative effects unique to modern times. Heroin is an
opium derivative and, as with any of the opium derivatives, there is a severe physical/mental
dependency that develops when Heroin is abused.
The Birth of the American Heroin Addict
In the mid to late 1800’s, opium was a fairly popular drug. Opium dens were scattered throughout what
we know today as the Wild West. The opium influx during this period was due in large part to the drug
being brought into the country via Chinese immigrants who came here to work on the railroads.
Accurate American history tells us that famous names of the period like Wild Bill Hickock and Kit Carson
actually frequented opium dens more often than saloons. The stereo-typed picture we have of the
cowhand belly up to the bar drinking whiskey straight after a long hard ride on the dusty trail is only
part of the story of the old west. Oftentimes the cowhand was not belly up to a bar at all. He was in a
prone position in a dim candle-lit room smoking opium in the company of an oriental prostitute. It was
not uncommon for some of these cowhands to spend several days and nights at a time in these dens in
a constant dream-state, eventually becoming physically addicted to the drug.
Nonetheless, it was true that alcoholism was a bigger problem. Alcoholism was one of the major sources of violence and death during this period.
Eventually, however, opium was promoted as a cure for alcoholism by the late 1800’s.
It was from opium that morphine, a derivative, was developed as a pain killer in approximately 1810. It was considered a wonder drug because it
eliminated severe pain associated with medical operations or traumatic injuries. It left the user in a completely numb euphoric dream-state. Because of
the intense euphoric side effects, the drug in 1811 was named after the Greek god of dreams, Morpheus, by Dr. F.W.A. Serturner, a German pharmacist.
By the mid 1850’s, morphine was available in the United States and became more and more popular with the medical profession. The benefits of using
the drug to treat severe pain was considered nothing short of remarkable to doctors of the time. Unfortunately, the addictive properties of the drug, on
the flip side, went virtually unnoticed until after the Civil War. Source For this Article
Simplicity is what made this 1980s-public service announcement—in which a man cracks an egg into a heated frying pan to illustrate the damage caused
by drugs—compelling. One plus one equals two. If you do drugs, they ruin your life. Period.
“This is your brain. This is drugs. This is your brain on drugs. Any questions?”
Yet in reality, drug addiction is not that simple.
A quarter of a billion people use illicit drugs annually. This is despite the increased risk of overdose,
which has gone up 33 percent in the United States over the last five years, according to the Centers
for Disease Control and Prevention.
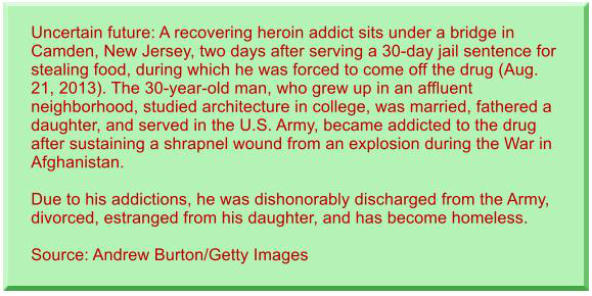
At the front end of increasing drug use is heroin, which is now the number-one killer among illegal
drugs. Given its resurgence over the past decade, the old stigma of it being confined to inner cities,
the poor, and minorities is fading. The highly addictive drug now grips rural towns and wealthier
suburbs.
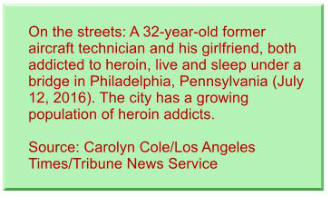
The story of an Ohio couple interviewed by The
Columbus Dispatch shows heroin abuse’s impact. The
39-year-old man, who became hooked on painkillers
after dislocating his shoulder, once dreamed of working in law enforcement. Instead, he became addicted
to the drug after he discovered that the $10 to get high from heroin is more sustainable than paying $80 per
pill for painkillers.
His girlfriend, who aspired to work in a veterinarian’s office, began her struggle with drug abuse after
accepting an OxyContin pill from her boyfriend. Their four children were eventually taken by authorities
and put up for adoption.
Twelve years or so into their addiction, the couple, now frail and haggard, spend their days scouring streets
and rummaging dumpsters for soda cans and other recyclables to sell to support their habit. On a good
day, they earn enough to split a dose of heroin the size of a watermelon seed.
“It just makes you feel more of what you are supposed to be,” the man explained in a video interview
posted by the newspaper. “I know there is normal, but this makes you feel above and beyond normal. It
makes you feel you can do way more than what you can.”
“It makes you feel like you are Superman…” he added.
This explains why the drug is so hard to kick—heroin
rewires the brain and makes you feel invincible. Brad
Lander, clinical director of addiction medicine at Ohio
State University’s Wexner Medical Center, explained in a
Columbus Dispatch article that heroin “changes the brain
and the user’s reality.”
He described how heroin activates the brain’s release of
adrenaline and endorphins—the body’s naturally
occurring “opiate system” that normally provides energy
and helps relieve pain when we get hurt. Once addicted, the brain thinks it needs heroin just to function.
“You need to have it, or you feel dysphoric, sad, anxious, depressed,” Dr. Lander continued. “Any pain
you have is exaggerated.”
He likened an addict being denied heroin to a person starving to death.
“If you’re starving to death, you’ll take more risks with employment and relationships. You would steal
more things if you were really starving to death. So [addicts] are doing things they never thought they
would do.”
This depiction of hopeless dependence has replicated itself across America—from bustling streets in downtown Seattle, Washington, to quaint fishing
towns in Massachusetts. As a result, those on the front lines are trying a new approach: Instead of focusing on stopping its usage, the fight has turned to
minimizing the drug’s effects.
In short, in the modern war on heroin, authorities are beginning to lay down their weapons.
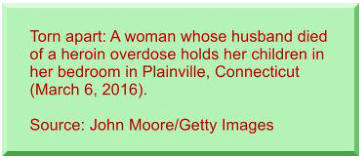
Ripple Effects
Technology has also played a role in putting a new face on the heroin crisis.
Last autumn, a picture of a couple who overdosed in the front seat of their SUV
made its way around social media. The most sickening part about the photo was the
blank stare of a four-year-old boy sitting in the back seat, who presumably witnessed
all that transpired. Authorities who released the photo did so on the grounds that “it
is time that the non-drug using public sees what we are now dealing with on a daily
basis” (STAT).
For many, the little face peering from the backseat of the car made heroin abuse more
real. Yet the photo was just a glimpse into what occurred at the scene. Reports
revealed that the distressing image was merely the finale of a death-defying spectacle.
Law enforcement officials recounted: “A school bus was making its way down St. Clair
Avenue, stopping now and then to let off children. The Ford Explorer was just behind
it, weaving erratically. Now, abruptly, the driver hit the brakes. The SUV skidded across
the pavement—narrowly missing the bus. It drifted at an angle onto Prospect Street
and came to rest near the spot where the children had disembarked, steps from a
church” (ibid.).
A police officer who witnessed the entire event reported that when he approached the vehicle the driver’s “head was bobbing back and forth. His pupils
were pinpricks. His speech was almost unintelligible.”
The officer says the man then reached for the gearshift and mumbled something about taking his
unconscious female passenger to the hospital. This prompted the officer to lean in and snatch the keys from
the ignition. While doing so, he noticed the boy in the back seat.
“At that moment,” the story continued, the driver “went completely unconscious” while the woman, “the
boy’s grandmother and legal guardian, was ‘turning blue.’”
After backup and medical support arrived, the picture was taken to use as evidence in court. The
photographer, a 24-year police force veteran, admitted that as he looked through the lens, he could not help
but to think of the child.
“He never said a word,” the photographer told the news outlet. “To this day I have not heard his voice.”
“Just seeing that blank, emotionless expression on his face—it spoke for itself,” he continued.
According to officials, heroin laced with fentanyl was to blame for the whole ordeal. Often
called heroin’s synthetic cousin, fentanyl is just one example of a trend in which users are
experimenting with more potent chemicals, leading to more overdoses and, sadly, more
deaths.
Examples of this are difficult to hear. A five-month old girl from Pennsylvania starved to death
in her crib after her parents, in their 20s, fatally overdosed on fentanyl. The coroner believes
the child survived alone in her bed for three or four days after her parent’s death before
eventually succumbing to a lack of food and water. All three bodies were discovered by a
neighbor.
Police and paramedics report that it is not unusual to get called to a residence where multiple
family members have overdosed. They say that such calls due to heroin and other powerful
opioids are mounting. In one community where overdose calls are twice the number of all other medical calls combined,carfentanil—an elephant
tranquilizer—is to blame.
The heroin-carfentanil concoction is so intense—10,000 times more powerful than morphine!—that it can take multiple doses of the heroin antidote
Narcan (or naloxone) to revive an overdose victim.
The cost to communities for this life-saving remedy is growing as the desire for an increased high spins out of control.
“A dose of Narcan would usually revive a person and bring them back. What we are noticing now is our paramedics sometimes use between four and six,
maybe seven doses of the Narcan to revive them, so it is a lot stronger and it has taken a lot more,” a police official told Fox 8 Cleveland.
Even after being revived, victims cannot seem to be scared out of overdosing again. One health official told STAT that he had witnessed people
overdose, be revived, then show up again the next day, blue in the face from another overdose.
One of the saddest parts, though, is the fact that many of them are parents, which, he said, seems irrelevant to those who are hopelessly hooked.
“When they are looking at their children, and their children are not enough to make them stop, what really can you say to them?” he told STAT.
These are just some of the awful details of what leaders and other official face. Addicts, no matter how hard they try, cannot get clean. Even those who
have gone months or years without abusing often fall back into the trap of dependence. Those charged with resolving the crisis are left to throw all sorts
of ideas at the wall in hopes of pinpointing a solution that finally sticks.
Harm Reduction
An emerging trend in combatting heroin addiction is to replace the traditional approach of abstinence—which involves a complete cessation of heroin
use by addicts—with that of “harm reduction.”
Two versions of this controversial approach are often used to combat abuse. One involves lessening the usage of the harmful substance with the goal of
slowly reducing dependence. The second involves decreasing the “surrounding effects” of drug addiction—without reducing the use of the harmful
substance itself.
Methadone clinics are a good example of the first version of harm reduction therapy. Methadone is a synthetic opiate shown to reduce heroin
withdrawal symptoms for 24 to 36 hours per dose. The medication, usually dispensed in liquid form, is taken once per day and only available through
licensed clinics. Those in treatment, which can go on for years, say that methadone drastically reduces their chance of relapse and is often the bridge
they need to slowly wean themselves off heroin.
But these clinics, which are beginning to treat those hooked to opioid-based pain meds as well, are not a panacea. Depending on the clinic’s location,
addicts may have to travel great distances to receive their daily dosage. And as the number of patients treated by clinics grows, addicts find it more
difficult to make treatment a part of their daily routines.
“Like the morning rush at a Starbucks cafe, cars, pickups and sport utility vehicles start packing into the Volunteer Treatment Center’s parking lots while
it’s still dark,” Times Free Press reported. “The clinic…opens at 5:30 a.m. seven days a week. Drug treatment clinics open early in the morning so that
patients can take their medicine before work. Patients line up inside the clinic and watch red and green lights over a row of private booths staffed by
licensed practical nurses.
“When one patient is done, the green light comes on and the next person
enters and closes the door…[Through] an opening in a window inside the
booth, the nurse hands over the methadone…in tablet or liquid form. The
nurse makes sure the patient downs the dose. Traveling to the clinic
every morning to take methadone isn’t convenient for most patients.”
Perhaps the biggest challenge with methadone clinics, however, is that
most people simply do not want them in their neighborhoods. There is a
negative stigma attached to having a drug clinic in the community and
most facilities are prone to loitering addicts who commit other crimes
such as theft.
Another harm reduction approach is known as Law Enforcement Assisted
Diversion (LEAD). According to the program’s website, it “allows law
enforcement officers to redirect low-level offenders engaged in drug or
prostitution activity to community-based services, instead of jail and
prosecution.”
Under the LEAD program, city government officials, police officers,
prosecutors and social workers work closely together to keep addicts out
of the criminal justice system. Participants receive food, clothing, shelter
and job training. Those administering the program say relapses are
expected.
Naturally, many are concerned that programs like LEAD enable addicts
and do not incentivize change. They assert the program stops just short
of the decriminalization of heroin. Proponents of the program say they
want to keep addicts safe until they are ready to change.
Another concern with LEAD is cost. The program started up with $4
million in private funding in the city of Seattle alone, which covered about 300 participants. Yet private money ran out in 2015, leaving taxpayers to fill the
gap. Opponents believe that implementing a similar program with many times this number of addicts across the country may not be sustainable.
At the far end of the harm reduction approach is the call for supervised heroin injection sites. This means users would take heroin at taxpayer-funded
facilities where a nurse would supervise—and be available to deliver an overdose antidote if necessary. Those promoting the program say the facilities
would offer clean needles and access to treatment and recovery programs.
These heroin injection sites, already implemented in Canada, Australia and parts of Europe, have received mixed reviews. A major problem is that facility
officials turn a blind eye to illegal drug use. There is also the risk of facilities being exposed to lawsuits in the case of death or serious injury.
Some government officials say it is worth the risk given all the ancillary problems associated with heroin addiction. They believe they can avoid many of
the necessary legal and political hurdles for approval if heroin addiction were to be designated an “epidemic” by state health officials.
Opponents remain adamant, however, that these supervised facilities are a bad idea.
“The goal here should be getting people off drugs, not doing what we can to make it easy for people to continue to do them,” an attorney and adviser
for Drug Free America Foundation, Inc. told Fox News.
Another panelist added: “In a way it is giving up on these heroin addicts, in the short term maybe they are giving up the dirty needles, but are they really
addressing the underlying cause of the addiction, figuring out a way to get sober?”
If you want to offer us your opinion, click on the button labeled My Opinion. Thank you.
April 17 2017
The drug in 1811 was named after the Greek god of dreams,
Morpheus, by Dr. F.W.A. Serturner, a German pharmacist.











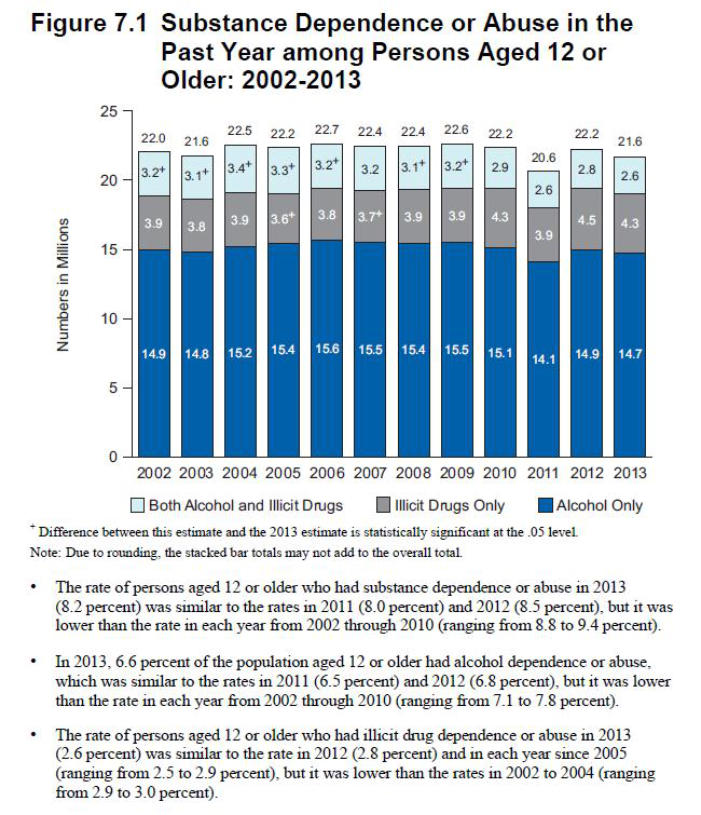
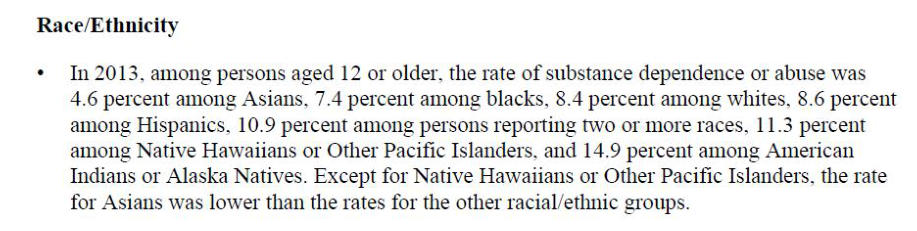
The following information was published through a report prepared by the
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Substance Abuse and Mental Health Services Administration
Center for Behavioral Health Statistics and Quality
The title of the report is:
Results from the 2013
National Survey on Drug Use and Health:
Summary of National Findings






You are invited to request from PVC the following documents in a PDF format:
Results from the 2013
National Survey on Drug Use and Health:
Summary of National Findings
And
drugs WHAT YOU NEED TO KNOW
Please send us an email note to Contact@PuraVidaCommunity.com requesting these two documents completely free of change.



